Migraine Relief Guide: How to Finally Stop Letting Headaches Control Your Life
Introduction
What Is a Migraine?
A migraine is not just a bad headache. This condition stems from abnormal neurological processes that disrupt normal brain function. Migraines, unlike typical headaches, often cause severe pain accompanied by nausea, sensitivity to light, and visual changes.
Key Characteristics of Migraine
- Throbbing pain: The headache often involves a pulsating sensation, which can vary from mild to intense and usually affects one side of the skull.
- Duration: Migraines typically last for 4-72 hours, much longer than typical headaches
- Symptoms: Nausea and vomiting are common digestive symptoms that occur during attacks
- Light and sound sensitivity: Need to retreat to dark, quiet spaces
- Gets worse with movement: Physical activity intensifies the pain
This complete guide covers migraine causes, symptoms, tests, and treatments to help you better manage living with migraines. Whether you are newly diagnosed or have been dealing with migraines for years, you will find practical information to help manage your condition better.
Stop Guessing – Get Your Personal Migraine Analysis
and medical history.
What Happens in the Brain During a Migraine?
Migraines involve a series of brain changes that lead to distinct symptoms. Below is a breakdown of the process, with each stage explained in a bit more detail:
Electrical Signal
A wave of electrical activity disrupts brain cells, starting the migraine process. This ripple effect sets off the entire chain of events.
Chemical Release
In response, the brain releases chemicals that act as messengers. These can increase the brain’s sensitivity, intensifying the migraine.
Blood Vessel Response
These chemicals cause blood vessels to expand or contract, altering blood flow. This shift is a key source of throbbing pain and discomfort.
Symptoms Appear
The final result is the onset of symptoms, which vary greatly. Effects can last for hours or even days depending on the individual and episode.
To understand how do you get a migraine and the detailed mechanism behind this complex neurological process, watch this video:
Video Credits: WebMD
What are the Different Types of Migraine?
Migraines are classified mainly into two types: Migraine without aura and Migraine with Aura, and each type has different forms based on the symptoms people experience. Understanding these types helps you identify your specific condition and find the right treatment approach.
Migraine Without Aura (Common Migraine)
Main Characteristics: Head pain occurs without warning, ranges from moderate to severe intensity, often includes nausea and sensitivity to light
| Subcategory | Description | Duration | Prevalence |
|---|---|---|---|
| Episodic Migraine | Less than 15 headache days per month | 4-72 hours per attack | Most common form |
| Chronic Migraine | 15+ headache days per month | Ongoing condition | 1-2% of population |
| Menstrual Migraine | Occurs 2 days before to 3 days after menstruation | 4-72 hours | 60% of women with migraines |
| Vestibular Migraine | Dizziness and balance problems | 5 min-72 hours | 1-3% of population |
| Abdominal Migraine | Stomach pain instead of headache | 2-72 hours | 0.2-4.1% of children |
Migraine With Aura (Classic Migraine)
Main Characteristics: Warning signs before headache, visual disturbances, tingling, and speech problems
| Subcategory | Description | Duration | Prevalence |
|---|---|---|---|
| Typical Aura | Visual and sensory symptoms followed by headache | 5-60 min (aura), 4-72 hrs (headache) | 20-25% of all migraines |
| Silent Migraine | Aura symptoms without headache | 5-60 minutes | 4-5% |
| Hemiplegic Migraine | Temporary weakness on one side | 4-72 hours | Less than 0.01% |
| Retinal Migraine | Vision loss in one eye | 5-60 minutes | Rare; data unknown |
How Common are Migraines: Migraine Statistics
Migraines are common. More than 1 billion people worldwide have migraines. It ranks as the 3rd most common illness.
Gender and Age Statistics:
- Women: About 18% of women get migraines, and since this happens three times more than in men, being female increases migraine risk.
- Men: 6% of adult men have migraines
- Peak age: 35-45 years old, with symptoms starting as early as 15 years old. Young adults (15-39) are the most affected group.
What are the Main Causes of Migraines?
Migraines are intense headaches that create a pounding sensation, usually on one side of your head. The pain occurs when nerves surrounding blood vessels in your brain become activated and send pain signals.
Primary Causes of Migraine
| Cause Category | Description |
|---|---|
| Genetic Factors |
|
| Stress |
|
| Hormonal Changes |
|
| Neurological Dysfunction |
|
| Vascular Changes |
|
| Environmental Factors |
|
What Triggers Migraines?
Triggers for migraines vary widely among individuals. Migraine attacks begin with triggers. Some of the common migraine triggers are:
Stress-Related Triggers
- Work pressure and deadlines
- Financial concerns
- Relationship conflicts
- Major life changes
Dietary Triggers
- Aged cheeses
- Processed meats with nitrates
- Alcohol (especially red wine)
- Chocolate
- MSG (monosodium glutamate)
- Artificial sweeteners
Sleep-Related Triggers
- Too little sleep (less than 7 hours)
- Too much sleep (more than 9 hours)
- Irregular sleep schedule
- Poor sleep quality
Hormonal Triggers
- Menstrual cycle fluctuations
- Pregnancy
- Menopause
- Birth control pills
- Hormone replacement therapy
Environmental Triggers
- Bright or flashing lights
- Strong odors or perfumes
- Weather changes
- Barometric pressure changes
- Loud noises
Uncover Your Hidden Migraine Triggers
How to Identify Migraine Triggers
Finding your personal migraine triggers requires careful observation and tracking over time. Here’s a complete approach:
Keep a Detailed Migraine Diary
Start recording every migraine episode for 30-90 days. Extended tracking helps reveal clearer connections between your lifestyle and headache patterns.
Track Daily Factors
Document food, sleep, stress, and weather every day, not just on migraine days. This helps you establish a baseline and see what’s different when a migraine occurs.
Note Timing with Weekly Reviews
Look at your diary each week to spot any obvious connections. Did a migraine consistently happen after a specific meal or a stressful day at work?
Identify Factors with Monthly Analysis
After a month, review all your data to find triggers that appear repeatedly. This broader view helps confirm patterns that might not be obvious week-to-week.
Test Trigger Elimination
Once you identify potential triggers, avoid them one at a time for 2-4 weeks each. This is the best way to confirm if they are a direct cause of your migraines.
Key Details to Document
- Date and time of onset
- Severity level (1-10)
- Duration of headache
- Associated symptoms
- Potential triggers (24-48 hrs prior)
- Menstrual cycle (for women)
- Sleep quality and hours
- Stress levels (1-10)
- Weather conditions
- Foods consumed
The key is consistency. Maintain your diary for a minimum of one month to identify reliable connections. Most people find their headaches result from multiple factors working together rather than individual causes.
Common Medical Conditions That Trigger Migraines
Hormonal Disorders
Thyroid:
Thyroid problems affect brain chemistry, whether overactive or underactive, affecting women 5 times more than men.
This condition creates hormonal chaos that frequently results in migraine attacks among women during their fertile years.
Estrogen:
Menopause triggers migraines when estrogen levels drop in women aged 45-55.
Adrenal:
Adrenal problems create stress hormone imbalances that disrupt sleep in high-stress professionals.
Sleep Disorders
Sleep apnea:
Sleep apnea reduces oxygen to the brain, causing inflammation that triggers migraines.
Insomnia:
Insomnia disrupts sleep patterns, making migraine attacks more frequent and severe.
Restless leg syndrome:
Restless leg syndrome disrupts deep sleep, causing frequent migraine attacks.
Shift Work Disorder:
Shift work disorder disrupts your body clock and may lead to frequent migraine attacks.
Narcolepsy:
Narcolepsy creates irregular sleep patterns, managed with scheduled naps and stimulants.
Mental Health Conditions
Depression:
Depression lowers brain chemicals that increase migraine risk by 2.5 times.
Anxiety:
Anxiety raises stress hormones, increasing migraine frequency by 60%
Bipolar disorder:
Bipolar disorder affects brain chemicals, making migraines 3 times more likely
PTSD:
PTSD keeps your stress response active, increasing migraine risk by 70%
Panic disorder:
Panic disorder causes stress hormone spikes, making migraines 2 times more common
Neurological Conditions
Epilepsy:
It affects brain electrical activity in ways that can trigger both seizures and headache episodes.
Stroke:
A previous stroke damages brain blood vessels, causing sudden, severe headaches
Tumors:
Brain tumors put pressure on brain tissue, causing headaches that get worse over time.
Multiple sclerosis:
It harms the protective covering of the nerves, often resulting in headache problems.
Injuries:
Head injuries disrupt brain chemistry, resulting in post-concussion headaches
Autoimmune & Inflammatory
Lupus:
Lupus causes body-wide swelling and sensitivity that affects brain blood vessels, leading to frequent, severe migraines.
Rheumatoid arthritis:
Rheumatoid arthritis creates ongoing inflammation throughout the body, making migraines more frequent.
Fibromyalgia:
Fibromyalgia makes the nervous system overly sensitive, making daily headaches common.
IBD:
Inflammatory bowel disease affects the gut-brain connection through inflammation, causing migraines during flares.
Celiac:
Celiac disease triggers inflammation from gluten, causing migraines after gluten exposure.
What are the Migraine Signs and Symptoms?
Migraine symptoms can vary from person to person, but they generally fall into two main categories: those with headache pain and those without. Recognizing these symptoms early helps you take action and manage your condition better.
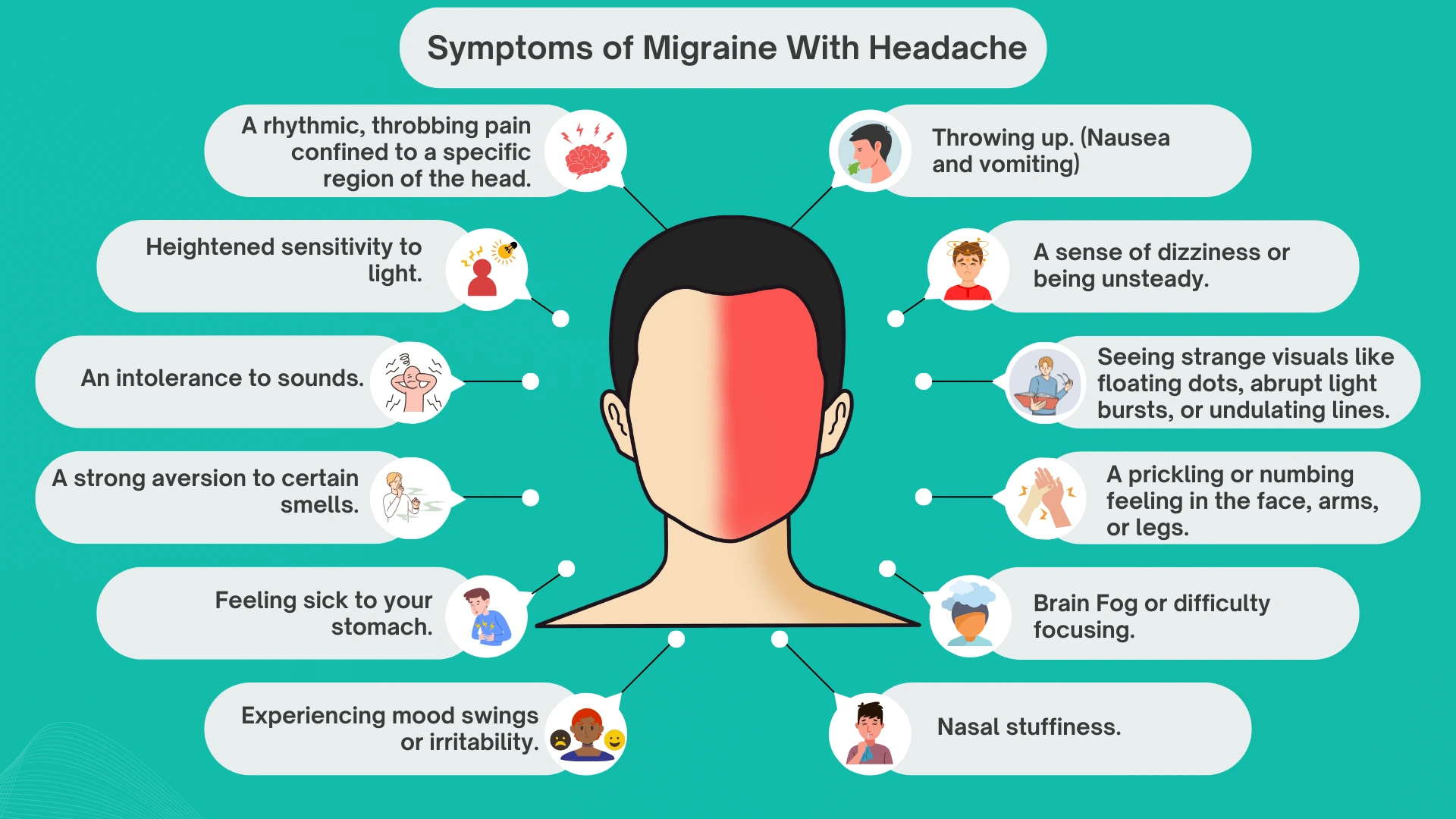
Symptoms of Migraine with Headache
- Head pain: A rhythmic, throbbing pain confined to a specific region of the head that intensifies with physical exertion
- Light and sound sensitivity: Heightened sensitivity to light and intolerance to sounds
- Nausea and vomiting: Feeling sick to your stomach and throwing up
- Smell aversion: A strong aversion to certain smells
- Dizziness and unsteadiness: A sense of dizziness or being unsteady
- Vision problems: Vision that is out of focus and seeing strange visuals like floating dots, abrupt light bursts, or undulating lines
- Numbness and tingling: A prickling or numbing feeling in the face, arms, or legs
- Cognitive difficulties: Brain fog, difficulty focusing, and struggling to articulate thoughts or select appropriate words
- Fatigue and weakness: A feeling of exhaustion or lack of strength
- Neck tension: A tight or sore neck
- Mood changes: Experiencing mood swings or irritability
- Food cravings: A strong desire for specific foods
- Increased urination: Needing to urinate more frequently
- Excessive yawning
- Nasal congestion: Nasal stuffiness
- Tinnitus: Hearing a ringing or buzzing sound
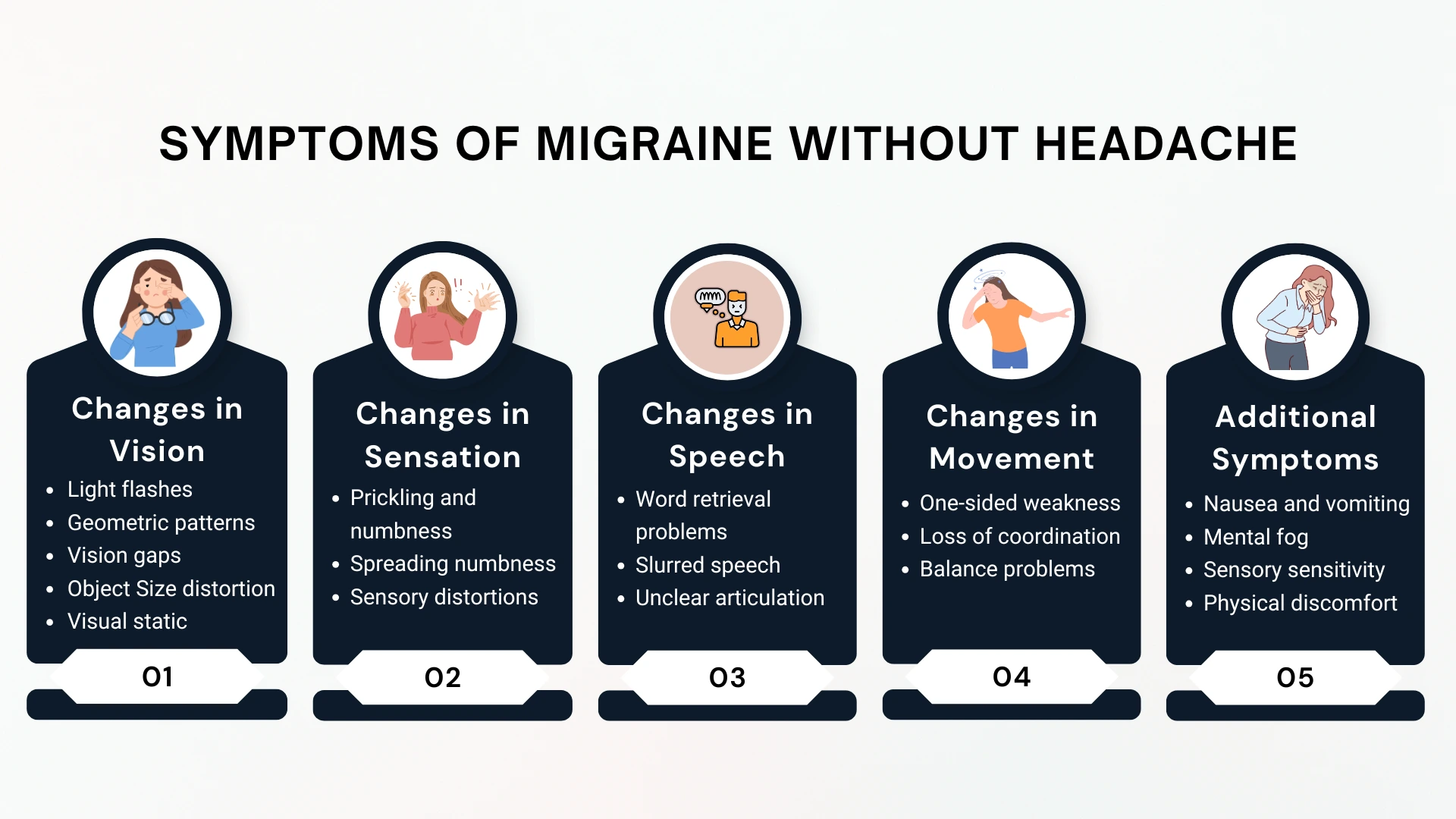
Symptoms of Migraine without Headache
- Changes in Vision:
- Light flashes, star-like dots, or shimmering spots
- Geometric patterns or zig-zagging lines
- Temporary blind spots or vision gaps
- Objects appearing larger or smaller than normal
- Visual static like TV snow
- Changes in Sensation:
- Tingling or numbness spreading from hands to face
- Altered smell, taste, or touch sensations
- Changes in Speech:
- Difficulty retrieving words.
- Indistinct or slurred speech patterns.
- Speaking in a mumbled or hard-to-understand way.
- Changes in Movement:
- Muscle weakness affecting half of the body.
- A loss of coordination or stability.
- Additional Signs:
- Nausea and vomiting
- Dizziness or spinning sensation
- Mental fog or confusion
- Sensitivity to light, noise, or odors
- Fatigue, chills, sweating, or nasal congestion
- Stomach pain
What Part of Your Head Hurts When You Have a Migraine?
The location of the pain depends on which branches of the trigeminal nerve are affected. This nerve is essential in migraines, as it carries pain signals between the brain and face, causing localized flare-ups.
Common pain locations:
- Temples – Most common area
- Forehead – Above one or both eyes
- Back of head – Occipital region
- Side of head – Unilateral pain
- Behind eyes – Deep, throbbing sensation
Duration of a Migraine Attack
- Standard Migraine: A common migraine headache attack may persist for a duration of 4 to 72 hours.
- Aura: The visual or sensory disturbances of an aura usually last between 5 and 60 minutes.
- Vestibular Migraine: Episodes of dizziness or vertigo can be as short as a few seconds or last for several days.
- Retinal Migraine: Temporary vision loss in one eye from a retinal migraine usually lasts for about 5 to 60 minutes.
- Status Migrainosus: In rare cases, a very severe migraine attack can last for more than 3 days. It is a pressing health issue that necessitates professional medical care.
How Do Doctors Test for Migraines?
| Test | Description |
|---|---|
| MRI (Magnetic Resonance Imaging) | If your headache symptoms are unusual or change suddenly, your doctor may order an MRI to check for serious problems like a brain tumor or stroke. |
| CT Scan (Computerized Tomography) | In an emergency, a CT scan can quickly show if a sudden, severe headache is from something like a brain bleed. |
| Blood Test | Your doctor might use a blood test to see if an infection or thyroid issue is causing your headaches. |
| EEG (Electroencephalogram) | If you lose consciousness during a migraine, an EEG can help your doctor figure out if a seizure disorder is the real cause. |
| Spinal Tap (Lumbar Puncture) | This test is only done if your doctor thinks your headache could be from a serious infection like meningitis or a problem with your spinal fluid. |
Migraine Diet Guide: What Can You Eat to Cure a Migraine?
Understanding the specific ways foods interact with your body is crucial for migraine management. This guide explains the mechanisms behind why certain foods can be beneficial, while others can act as triggers for a migraine attack.
What is Good to Eat When You have a Migraine?
Magnesium-Rich Foods
Magnesium is crucial for proper nerve and muscle function. It may prevent migraines by calming overexcited nerves in the brain, blocking pain-transmitting chemicals, and counteracting the wave of brain cell activity (cortical spreading depression) associated with migraine aura.
Food Examples:
Leafy greens (spinach, kale), Nuts and seeds (almonds, pumpkin seeds), Legumes (black beans, lentils)

Omega-3 Fatty Acids
Migraine is a result of inflammation of blood vessels and nerves of the brain. Omega-3s have powerful anti-inflammatory properties that help produce compounds to reduce this inflammation and lessen pain.
Food Examples:
Fatty fish (salmon, mackerel, sardines), Seeds (flaxseeds, chia seeds), Walnuts

Riboflavin (Vitamin B2)
Migraines are associated with a decrease in energy production within brain cells. Riboflavin is key for cellular energy metabolism, which can make brain cells more resilient to migraine triggers.
Food Examples:
Eggs, Lean meats (chicken, turkey), Dairy products (milk, yogurt)

Proper Hydration
Insufficient fluid intake can lower the body’s total blood volume. As a result, the brain might receive diminished blood flow, a condition that can aggravate sensitive nerves and initiate a migraine. Maintaining adequate water intake prevents this.

Which Foods Trigger Migraines?
Aged Cheeses
The aging of cheese involves the breakdown of proteins, which results in the formation of tyramine. This compound causes blood vessels to constrict and then rapidly expand, a process that is a direct trigger for head pain in sensitive individuals.
Food Examples:
Blue cheese, Cheddar, Parmesan, Feta

Processed Meats
Preservatives like nitrates and nitrites in these meats are converted to nitric oxide in the body. Nitric oxide is a potent vasodilator (it widens blood vessels), and this sudden expansion in the brain can start a migraine.
Food Examples:
Hot dogs, Bacon, Sausages, Deli meats

Caffeine
Your body gets accustomed to caffeine’s vessel-constricting effects. Consuming too much or missing a regular dose disrupts this balance and can cause a rebound effect where blood vessels expand, leading to a migraine.
Sources:
Coffee, Tea, Energy drinks
Alcohol
Alcohol is a diuretic that causes dehydration. It also acts as a vasodilator, which increases the blood flow to the brain. Red wine is a common culprit as it also contains tannins and can stimulate the release of migraine-inducing chemicals.
Sources:
Red wine, Beer, Other alcoholic beverages

MSG (Monosodium Glutamate)
As an excitotoxin, MSG can overstimulate glutamate receptors on nerve cells. Such overstimulation is capable of starting a domino effect of nerve impulses that begins the migraine sequence.
Commonly found in:
Packaged snacks, Canned soups, Restaurant food

Artificial Sweeteners
For sensitive individuals, the breakdown of artificial sweeteners like aspartame in the body can disrupt the balance of key brain chemicals, potentially leading to a migraine attack.
Commonly found in:
Diet sodas, “Sugar-free” products

Get Your Custom Anti-Migraine Nutrition Plan
your food preferences and trigger sensitivities.
Home Remedies for Migraine Relief
Simple home remedies for relief during an attack:
- Cold Compress: A cold pack applied to the forehead or neck can induce a numbing effect and constrict blood vessels, potentially easing throbbing discomfort. For more targeted relief, specialized migraine caps/hats offer 360-degree cold therapy coverage around the entire head. These gel-filled caps can be chilled in the freezer and provide hands-free cold compression, making them more convenient than traditional ice packs. Most migraine caps are reusable and can also be heated in the microwave for warm therapy if preferred.
- Dark, Quiet Room: Seeking refuge in a dark, silent area reduces sensory stimulation, which can soothe an overactive brain and lessen migraine symptoms.
- Gentle Scalp Massage: Gently pressing on your scalp and temples can help loosen tight muscles and boost blood flow, providing temporary comfort from the discomfort.
- Mindful Breathing: Deep, controlled breathing exercises can promote relaxation and help you manage the sensation of pain by calming your nervous system.
- Stay Hydrated: Slowly sipping water can alleviate migraine intensity if dehydration is a contributing factor, as it helps restore proper fluid balance.

Instant Migraine Relief at Home
Swift action can help prevent a migraine from intensifying or shorten its duration:
- Recognize Early Symptoms: Act quickly at the first signs (aura, mood changes, neck stiffness).
- Find a Calm Space: Retreat to a light/sound-controlled environment immediately.
- Warm Compress (Neck): Relaxes tense neck muscles.
- Consider Ginger: It helps with nausea, which is often accompanied by migraines.
- 4-7-8 Breathing: Inhale 4, hold 7, exhale 8 to promote relaxation.
- Limit Physical Activity: Avoid strenuous movement to prevent worsening pain.
Evidence-Based Natural Remedies for Migraine Prevention
| Supplement/Herb | Daily Dose | How It Works to Prevent Migraines |
|---|---|---|
| Magnesium | 400-600 mg | Your brain needs magnesium to work optimally. When you don’t have enough, nerve cells become overactive and trigger migraines. Magnesium soothes overactive nerve cells and relaxes tight muscles and blood vessels. |
| Riboflavin (Vitamin B2) | 400 mg | Brain cells need energy to function well. Riboflavin helps cells produce more energy and utilize oxygen more efficiently. Brain cells with an adequate energy supply don’t release the pain messages that cause migraines. |
| Coenzyme Q10 (CoQ10) | 300 mg | This helps your brain cells make energy more efficiently. It also protects brain cells from damage. When brain cells are healthy and have sufficient energy, migraines occur less frequently and are less severe. |
| Feverfew | 100-125 mg | This herb reduces the production of chemicals such as prostaglandins, CGRP, and substance P that cause inflammation. It also keeps pain-controlling brain chemicals like serotonin at healthy levels. This terminates the pain messages that trigger migraines. |
| Butterbur | 75 mg (PA-free extract) | Butterbur decreases inflammation in the blood vessels of your head. When blood vessels aren’t swollen or tight, they don’t trigger migraine pain. |
| Omega-3 Fatty Acids | 1-2 g | These healthy fats reduce swelling throughout your body, including in your brain. They also improve blood vessel function and strengthen cell membranes. Less swelling means fewer migraine triggers. |
| Melatonin | 3-9 mg | This natural hormone improves the quality of sleep and controls your body’s internal clock. Poor sleep and disrupted sleep patterns often trigger migraines. Better sleep means fewer migraine attacks. |
| Alpha Lipoic Acid | 300-600 mg | This powerful antioxidant protects brain cells from damage caused by harmful substances. It also boosts how well brain cells create energy. Well-protected and properly functioning brain cells rarely cause migraine attacks. |
| Ginger | 250-500 mg | Ginger blocks the body’s inflammation pathways. It also prevents the nausea and vomiting commonly experienced during migraines. By lowering inflammation and blocking pain messages, it helps stop migraine episodes. |
| Probiotics | 1-10 billion CFUs | Your gut and brain are connected. A well-functioning gut delivers beneficial messages to your brain. Probiotics support a healthy gut environment, which decreases the inflammation in the brain and reduces migraine triggers. |
Please Note:
- Always talk to your doctor before taking any supplements
- Some herbs can mix badly with your medicines
- Only use butterbur that says “PA-free” on the label
Create Your Complete Migraine-Free Life Plan
all designed for your unique needs.
What are the Best Migraine Medications?
Doctors prescribe different types of migraine medication based on your symptoms, frequency, and medical history. The main categories include acute treatments (for active attacks) and preventive medications (to reduce frequency).
Migraine Medications List
| Medication Type | Used For | How It Helps | Common Examples |
|---|---|---|---|
| Triptans | Acute moderate to severe migraine | Narrows blood vessels and block pain signals. First choice, works for 70% of people | Sumatriptan, Rizatriptan, Naratriptan |
| CGRP Antagonists | Acute/Prevention | Blocks CGRP protein that causes migraine | Rimegepant, Ubrogepant, Atogepant |
| CGRP Monoclonal Antibodies | Chronic migraine prevention | Blocks CGRP protein to prevent migraine attacks. 50% reduction in migraine days | Aimovig, Ajovy, Emgality, Vyepti |
| Botox Injections | Chronic migraine prevention | Blocks nerve signals that trigger migraines; Takes 2-3 treatment cycles to see full benefit and reduces migraine days by 50% in most patients | Botulinum toxin type A |
| Ergot Alkaloids | Acute severe migraine | Constricts blood vessels in the brain | Dihydroergotamine, Ergotamine |
| Beta-blockers | Prevention | Reduces nerve sensitivity and stabilizes blood vessels | Propranolol, Metoprolol |
| Anticonvulsants | Prevention | Calms overactive nerve cells | Topiramate, Valproic acid |
| Antidepressants | Prevention | Balances brain chemicals and pain signals | Amitriptyline, Nortriptyline |
What are the New Drugs for Migraine Headaches? Latest 2025 Advances
| Medication | Used For | Purpose & Mechanism | Common Examples |
|---|---|---|---|
| CGRP Nasal Spray | Acute migraine | Fast-acting CGRP blocker delivered through nose, works in 15 minutes | Zavzpret (zavegepant) |
| Oral CGRP Prevention | Daily prevention | Blocks CGRP daily to prevent migraines from starting | Atogepant (Qulipta) |
| Dual-use CGRP | Acute + Prevention | Can treat active migraine AND prevent future ones | Rimegepant (Nurtec ODT) |
| Combination Therapy | Acute migraine | Combines NSAID with triptan for enhanced effectiveness | AXS-07 (meloxicam + rizatriptan) |
Latest Research Findings:
A recent study highlights that the medication atogepant (Qulipta) shows the potential to provide immediate benefits for migraine prevention. According to the research, published on December 23, 2024, in Neurology, the medical journal of the American Academy of Neurology, this offers a significant advantage over older preventive medications that typically take weeks to show results. The findings suggest that atogepant may begin working almost right away for individuals seeking to prevent migraine attacks.
What is Surgery for Migraines?
Millions of people suffer from chronic migraines that don’t respond to traditional treatments. When medicines do not work, nerve decompression surgery offers better chances for people suffering from chronic migraine.
When is Surgery Required for Migraines?
- Neurologist diagnosis – Has been seen by a neurologist and diagnosed with migraine disease.
- Failed medical treatments – Tried multiple preventive medications without success
- Chronic migraine pattern – At least 15 headache days per month for 3+ months
- Identifiable trigger points – Specific nerve compression sites identified
- Positive response to nerve blocks – Temporary relief from diagnostic injections
Nerve Decompression Surgery for Migraine
Different types of surgery target different areas of your head where nerves get squeezed. Your doctor will choose the right surgery based on your pain location. About 9 out of 10 people who are good candidates for surgery see major improvement. This means their migraines either go away completely or get at least 50% better.
| Surgery Name/Nerve Involved | How It Helps Your Migraines | Success Rates |
|---|---|---|
| Frontal Nerve Decompression (Supraorbital nerve) | Reduces pressure on the nerve that causes forehead and eyebrow pain | 90% success rate in ideal candidates |
| Temporal Nerve Decompression (Temporal branch of trigeminal nerve) | Relieves nerve compression that triggers pain in temple area | 90% success rate in select patients |
| Occipital Nerve Decompression (Greater occipital nerve) | Frees up the nerve at back of head that causes neck-related migraines | 88.8% overall efficacy (8/9 cases) |
| Lesser Occipital Nerve Surgery (Lesser occipital nerve) | Stops nerve irritation that causes pain behind the ears and upper neck | 90% positive response, 69% complete recovery |
| Nasal Trigger Point Surgery (Sphenopalatine ganglion) | Addresses nerve problems inside the nose that can trigger migraines | Combined with other sites for optimal results |
| Combined Multi-site Surgery (Multiple nerve sites) | Treats several compressed nerves at once for complex migraine patterns | 94% of participants reported complete or significant improvement |
| Auriculotemporal Nerve Surgery (Auriculotemporal nerve) | Relieves nerve pressure near the ear that causes side-head migraines | 85-90% improvement in temporal migraines |
When Should You be Concerned About a Migraine?
Most people with migraines can handle their symptoms at home with proper care. However, some situations need medical help to prevent serious health problems.
See a doctor if you have:
- A headache that comes on suddenly and feels much worse than any you’ve had before
- Problems with speaking clearly or understanding others
- Loss of balance or trouble walking normally
- Changes in your vision that are new or different
- Feeling confused or having trouble thinking clearly
- Headache pain along with a high fever and neck stiffness
- Headaches that stop you from doing your daily tasks
- Pain episodes happening more than twice each week
- Your usual headache treatments stop working effectively
- Headache patterns that have changed from what’s normal for you
- Symptoms that worry you or seem different than before
Take Control of Your Migraines Today
that addresses root causes for lasting wellness improvements.
FAQs: Your Common Questions Answered Here
A migraine is characterized by a severe, pulsating headache that is often confined to one side of the head. This condition is frequently accompanied by nausea, along with a heightened sensitivity to light (photophobia) and sound (phonophobia). In contrast, tension headaches are generally less intense, impact both sides of the head, and typically do not lead to nausea or visual disturbances.
A migraine attack typically unfolds in four distinct phases:
Prodrome: Initial symptoms, such as mood alterations or fatigue, can appear 24 to 48 hours before the headache.
Aura: This stage is characterized by transient neurological symptoms, which include visual or sensory changes.
Headache: The primary phase is marked by considerable pain.
Postdrome: A recovery phase that is often likened to a “migraine hangover.”
Visual phenomena that occur during the aura phase of a migraine are known as migraine hallucinations. These can manifest as flashing lights, zigzag lines, or temporary blind spots, and they generally last for 5 to 60 minutes before the onset of the headache.
A typical migraine headache can persist for anywhere from four hours to three days. It is recommended to seek medical advice if a migraine attack extends beyond three days or if you experience three or more migraines within a week.
A migraine is said to have concluded when the headache pain has fully resolved and you have transitioned into the postdrome phase. Following the cessation of pain, you may continue to feel weary, sore, mentally foggy, or sensitive to light. These are called postdrome symptoms.
Females are three times more prone to experiencing migraines than males. Their episodes are frequently longer, more intense, and necessitate more medication. Hormonal shifts associated with menstruation, pregnancy, and menopause play a significant role in this increased prevalence among women.
Common Types in Women:
Menstrual Migraines are associated with hormonal fluctuations.
Migraine with Aura: More prevalent in women.
Chronic Migraine: Happening on 15 or more days per month.
Common Types in Men:
Cluster Headaches: More prevalent in men.
Migraine without Aura
Exercise-Induced Migraines
Physical activity can precipitate a migraine.
Children are also susceptible to migraines. Their migraines are generally of a shorter duration, lasting from 1 to 4 hours, and may present with more pronounced abdominal pain, nausea, and vomiting than head pain. Children often find relief after sleeping.
Common Types in Children:
Migraine without Aura: The most frequent type in children.
Tension Headaches: Frequently triggered by stress or academic pressures.
Abdominal Migraines are identified by stomach pain in the absence of a headache.
Cluster Headaches: Infrequent and mainly observed in boys over the age of 10.
Both emotional and physical stress are among the most widely cited triggers for initiating a migraine episode.
In some cases, milk can act as a migraine trigger. It is advisable to maintain a food journal to ascertain if dairy products are a trigger for your migraines.
1. Seek refuge in a dark, quiet room.
2. Place a cold compress on your head and a hot compress on your neck for 15 minutes. A migraine cap or hat may be used for added convenience.
3. Consume water slowly, as dehydration can exacerbate migraines.
4. Engage in deep breathing exercises to promote relaxation and alleviate tension.
5. Perform gentle stretches of your neck muscles to ease tension and stiffness.
To mitigate eye pain during a migraine, it is helpful to wear sunglasses, remain in a dimly lit environment, and apply a cold compress over closed eyes. It is also recommended to refrain from looking at screens.
Some individuals find relief through complementary therapies such as acupuncture, biofeedback, massage, yoga, meditation, or herbal remedies like butterbur and feverfew. It is important to consult with a healthcare professional before starting any of these alternative treatments.
How to deal with chronic migraines?
Chronic migraine is identified when an individual experiences headache symptoms on a minimum of 15 days per month for at least three months, with at least 8 of these days exhibiting migraine characteristics such as nausea, sensitivity, or aura. The management of chronic migraines entails a multifaceted approach that includes preventive medications, lifestyle modifications, stress management techniques, and ongoing collaboration with a neurologist.
Although severe migraine attacks are seldom a direct cause of stroke, research has indicated a marginally elevated risk of stroke, especially for those who have migraine with aura. It is essential to seek immediate medical attention if you experience a sudden, intense “thunderclap” headache, unexplained weakness, or abrupt speech difficulties.
While there is no definitive cure for migraines, they are eminently treatable and manageable. Through appropriate treatment, lifestyle adjustments, and effective trigger management, many individuals can substantially decrease the frequency and intensity of their migraine attacks.

