Living with PCOS: A Complete Guide to Symptoms, Diet, and Treatments
Introduction
What is PCOS?
PCOS (polycystic ovary syndrome) is a hormonal disorder many women face that occurs when the body produces too many male hormones (androgens). This imbalance can cause:
1. Missed periods
2. Skin troubles like acne and oily skin
3. Unwanted hair growth (hirsutism)
Despite its name, polycystic ovary syndrome doesn’t always include ovarian cysts – those small fluid sacs that can develop on the ovaries. PCOS disease affects how the body handles insulin and sugar, which explains why weight gain often comes with it. This guide covers the causes, symptoms, natural cure, and treatment for PCOS and
How Common is PCOS?
As of 2025, polycystic ovary syndrome is one of the most widespread hormonal imbalance conditions that affects women. It is estimated that about 8-13% of women globally experience the condition, which translates to approximately 1 in 10 women. Health organizations estimate that, in the United States, over 5 million women are impacted by PCOS.
Studies suggest that 50%-75% of women with PCOS remain unidentified. The diverse range of symptoms makes it difficult to recognize, with some women having only mild signs and symptoms. It often leads to delayed diagnoses, with many women finding out they have PCOS when trying to conceive or when other hormone-related health issues arise.
At What Age Does PCOS Start?
Polycystic Ovary Syndrome typically begins during adolescence, often around puberty, with many teenagers showing first symptoms as early as age 11. However, diagnosis frequently comes later in life. While PCOS can develop at any age, early detection leads to better management of symptoms and prevention of long-term health complications.
| Age Range | % of Diagnoses | Notes |
|---|---|---|
| 11-19 | About 25% | Early diagnosis usually happens when symptoms are obvious or a family history exists |
| 20-29 | About 50% | Early diagnosis usually happens when symptoms are obvious or a family history exists |
| 30-39 | About 20% | Later diagnosis, sometimes after years of unexplained symptoms |
| 40+ | About 5% | Less common but possible, especially with milder symptoms |
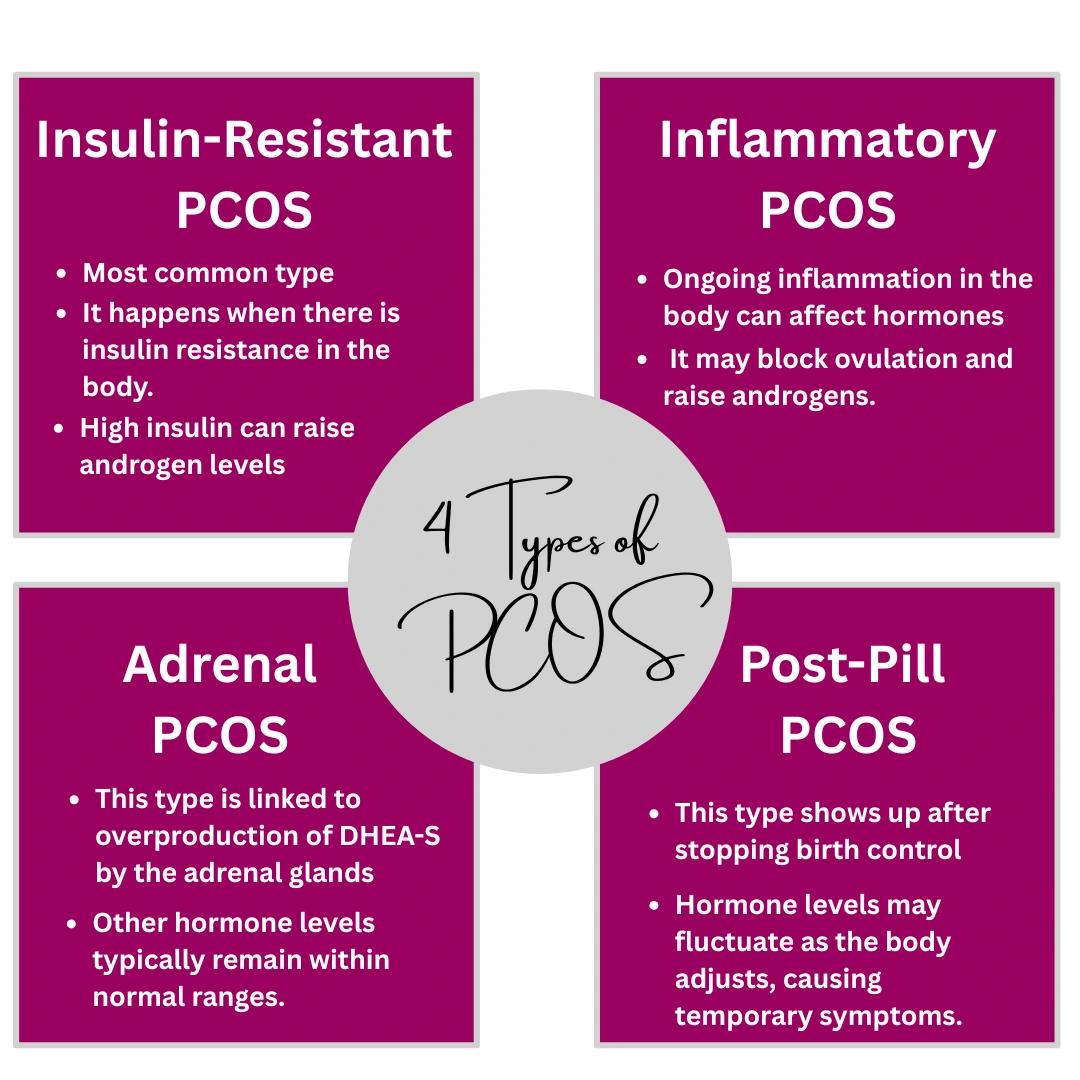
What are the types of PCOS?
Not all cases of Polycystic Ovary Syndrome are the same. Experts now describe four common types based on what causes the symptoms:
1. Insulin-Resistant PCOS: This is the most common type. It happens when there is insulin resistance in the body. High insulin can raise androgen levels, leading to disrupted ovulation.
2. Post-Pill PCOS: This type shows up after stopping birth control. Hormone levels may fluctuate as the body adjusts, causing temporary symptoms.
3. Inflammatory PCOS: Ongoing inflammation in the body can affect hormones. It may block ovulation and raise androgens.
4. Adrenal PCOS: This type is linked to overproduction of DHEA-S by the adrenal glands, while other hormone levels typically remain within normal ranges.
Each type requires a different treatment approach. Knowing your PCOS type can help you find the right treatment, from managing insulin to reducing stress or inflammation.
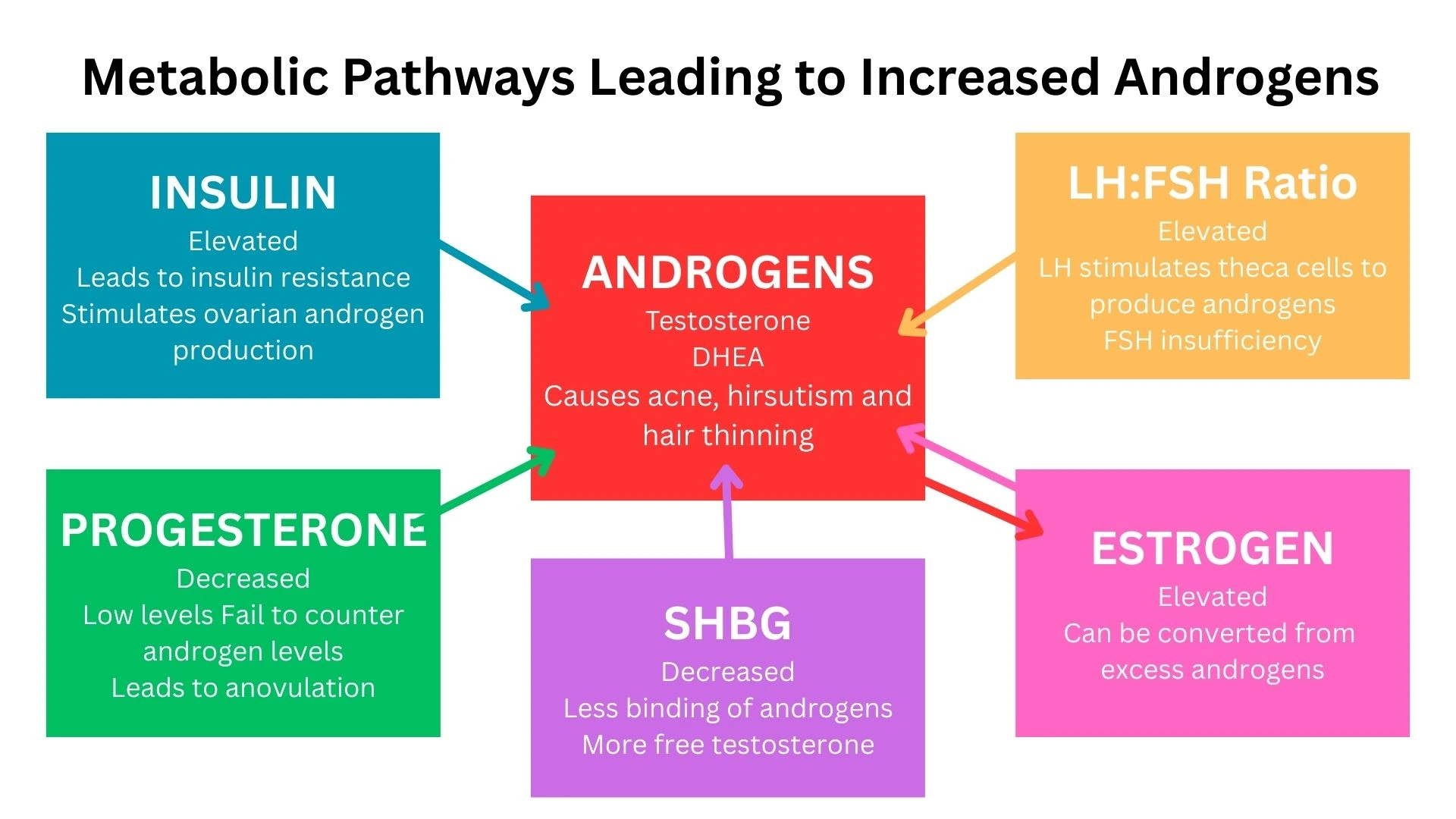
What Hormones are involved in PCOS?
In women with PCOS, several hormones are typically either too high or too low:
Insulin
Women with PCOS often have high insulin levels, which can lead to insulin resistance. In this condition, the body doesn’t use insulin effectively, triggering the ovaries to produce excess androgens (male hormones).
Androgens (Testosterone and DHEA)
High levels of testosterone and other androgens contribute to symptoms like hirsutism (unwanted hair growth), acne, and thinning hair. The levels of testosterone are often elevated in women with PCOS compared to those without.
Estrogen
Estrogen dominance invariably occurs with this condition, but the body often has trouble balancing this hormone due to the lack of ovulation, which can lead to irregular menstrual cycles and an increased risk of endometrial cancer.
Progesterone
Low progesterone levels commonly occur in PCOS, often due to the absence of ovulation, which can lead to irregular or entirely missed cycles.
LH (Luteinizing Hormone)
A common hormone imbalance in PCOS involves more LH (luteinizing hormone) compared to FSH (follicle-stimulating hormone). This uneven ratio can disrupt ovulation and may lead to the development of ovarian cysts.
What Causes PCOS?
The main cause of PCOS (Polycystic Ovary Syndrome) isn’t fully understood, but several key factors play a role.
1. Hormonal Imbalance
One of the main causes of PCOS is a disruption in hormone regulation. In women with this condition, the ovaries often produce excess androgens due to hormonal signals from the brain and high insulin levels. This imbalance interferes with the normal development and release of eggs during ovulation, contributing to the overall etiology of PCOS.
2. Insulin Resistance
A major factor in many cases is insulin resistance. When the body can’t use insulin well, it produces more of it. High insulin levels can prompt the ovaries to produce more androgens, further upsetting hormone balance.
3. Genetics
PCOS can run in families, so genetic factors are also believed to contribute to its etiology. If a mother or sister has it, the chances of developing it are higher.
4. Low-Grade Inflammation
Some women with PCOS may experience chronic, mild inflammation, which can signal the ovaries to make more androgens, further disrupting hormonal balance and adding to the causes of PCOS.
5. Pituitary Gland & Brain Signals
In rare cases, PCOS may be caused by the pituitary gland. Abnormal signals from the brain can lead to higher levels of LH (luteinizing hormone), which also encourages excess androgen production.
6. Medications like Depakote
Medications like Depakote can affect how the brain signals the ovaries by altering levels of certain brain chemicals, such as gamma-aminobutyric acid (GABA), which regulates hormone levels. This disruption has been linked to hormone changes and can cause PCOS-like symptoms in some women.
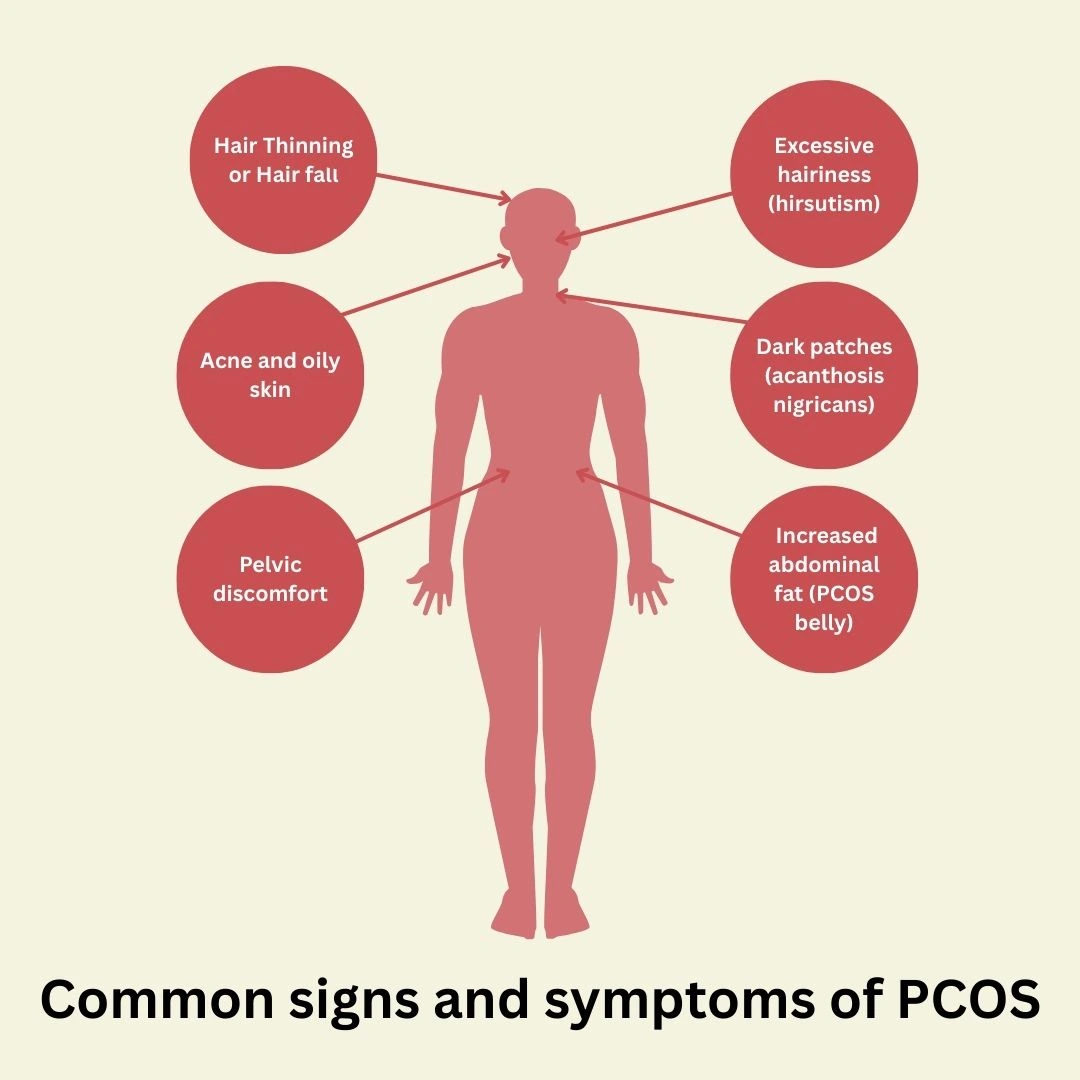
What are the PCOS Symptoms?
Polycystic Ovary Syndrome (PCOS) has a different appearance in each woman. This section highlights the most common signs and symptoms of PCOS, helping you identify the condition early.
1. An increase in abdominal fat, particularly around the belly area, which is particularly difficult to lose (known as PCOS belly)
2. Excessive hairiness due to a surge in androgen levels, particularly in areas like the face, chest, and back.
3. Hair thinning or hair fall from the scalp.
4. Acne or excessive greasy and oily skin, which commonly affects areas like the face, chest, and upper back of the body
5. Dark patches on the skin usually appear around the neck, groin, or underarms (called acanthosis nigricans).
6. Mood changes, such as anxiety or depression. Extreme moods swing, like irritability, and sometimes PMS is also noted in women suffering from this condition.
7. Fatigue or low energy: A lesser-known but common symptom in many women.
8. Pelvic discomfort or pain
9. Trouble conceiving: PCOS is a major contributor to infertility because it often leads to irregular ovulation, making it difficult to conceive.
10. Poor sleep or feeling tired even after sleeping. Brain Fog can also occur.
How is PCOS Diagnosed?
If you suspect you might have Polycystic Ovary Syndrome, getting a proper diagnosis is the first step in managing the condition. Here’s how PCOS is generally diagnosed:
1. Medical History and Symptoms Review
The first step in diagnosing PCOS typically involves a detailed conversation with your healthcare provider about your medical history. They will ask about your menstrual cycle, any irregularities you’ve noticed, and other symptoms like acne, excessive hair growth, and weight gain. These questions help doctors understand the scope of your symptoms and rule out other conditions.
2. Physical Examination
To gain further insights, your doctor may also perform a physical examination to look for signs of PCOS, such as excess facial or body hair (hirsutism), skin issues, or weight changes. They might also assess your abdomen for any pelvic discomfort or signs that could suggest ovarian cysts.
3. Blood Tests
Blood tests are essential for diagnosing PCOS. These tests measure hormone levels, especially:
1. Testosterone (high levels can indicate PCOS)
2. Insulin (to check for insulin resistance)
3. Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) (an imbalance can suggest PCOS)
These tests help determine whether there is a hormonal imbalance commonly associated with polycystic ovary syndrome.
4. Ultrasound
One of the most reliable ways to confirm a PCOS diagnosis is through an ultrasound. Your doctor may use a transvaginal ultrasound to inspect the ovaries for cysts. While cysts aren’t always present in every woman with PCOS, many people diagnosed with the condition show enlarged ovaries that contain multiple small cysts.
5. Excluding Other Conditions
Since many symptoms overlap with other conditions, your doctor may also conduct tests to rule out other possibilities, such as thyroid disorders, endometriosis, or pituitary gland disorders.
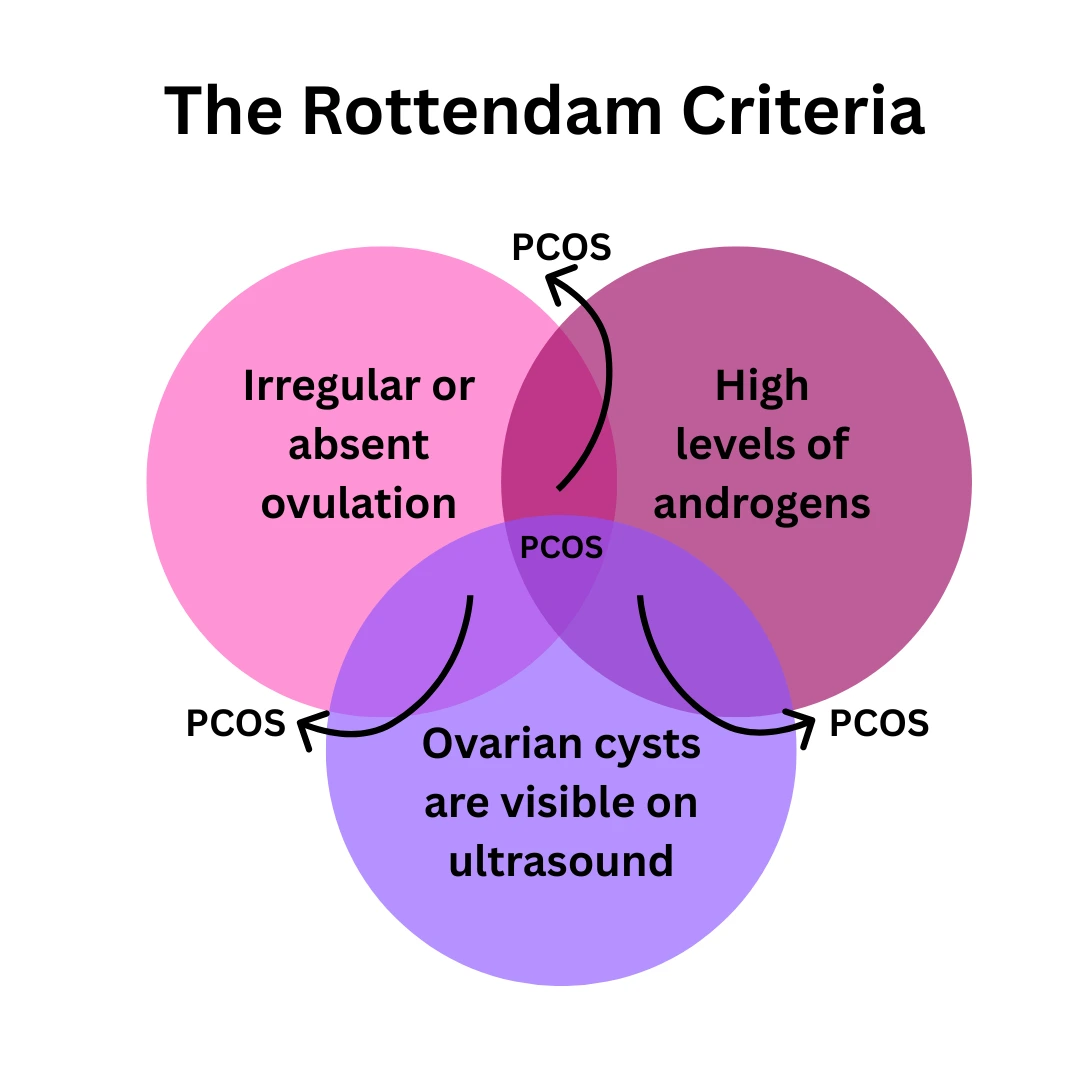
6. The Rottendam Criteria
To meet the diagnostic criteria for PCOS, a woman must present at least two out of three of the following conditions, according to the Rotterdam Criteria:
1. Irregular or absent ovulation (e.g., irregular periods)
2. High levels of androgens (male hormones)
3. Ovarian cysts are visible on ultrasound.
PCOS Diet Plan: What to Eat and Avoid for Better Health
Managing Polycystic Ovary Syndrome through diet is one of the most effective ways to reduce symptoms like irregular periods, acne, weight gain, and hair growth. While there is no one-size-fits-all approach, the right foods can help balance hormones, support insulin sensitivity, and improve fertility. Here’s your go-to guide for a PCOS-friendly diet that’s easy to follow and delicious!
What to Eat on a PCOS Diet?
| Food Type | Examples |
|---|---|
| Low Glycemic Index (GI) Foods | Whole grains (quinoa, oats, brown rice), Legumes (lentils, chickpeas, beans), Non-starchy vegetables (broccoli, spinach, zucchini) |
| Healthy Fats | Avocados, Nuts and seeds (almonds, chia seeds, flaxseeds), Oily fish (salmon, mackerel) |
| Lean Proteins | Chicken and turkey (skinless), Tofu and tempeh, Fish (tuna, salmon) |
| Fiber-Rich Foods | Whole fruits and vegetables (berries, apples, carrots, leafy greens), Legumes (beans, peas, lentils), Whole grains (brown rice, oats, quinoa) |
| Antioxidant-Rich Foods | Berries (blueberries, strawberries, raspberries), Leafy greens (kale, spinach), Nuts and seeds (walnuts, flaxseeds) |
| Dairy Alternatives | Almond milk, Soy milk, soy-based yogurt, Coconut milk, Coconut yogurt |
What to Avoid in a PCOS Diet?
| Food Type | Examples |
|---|---|
| Refined Carbohydrates and Sugars | Sweets (cookies, cakes, candy, sugary snacks), White bread, pasta, and other refined grains |
| Fried Foods | French fries, fried chicken, and deep-fried snacks |
| Processed Foods and Junk Food | Packaged snacks, chips, processed meats (bacon, sausage) |
| Excessive Dairy | Full-fat milk, cheese, and butter (if they worsen acne or digestive issues) |
| Caffeine (In Excess) | Coffee, energy drinks (opt for herbal teas instead) |
Best Supplements for PCOS: Natural Ways to Heal from Within
Polycystic Ovary Syndrome (PCOS) affects many women, but the good news is that treating PCOS naturally is absolutely possible—and in many cases, life-changing. While there may not be a one-size-fits-all permanent cure for PCOS, certain natural supplements for PCOS can support your hormones, reduce symptoms, and help you feel more like yourself again.

Inositol (Myo-Inositol + D-Chiro Inositol)
1. Supports ovulation and fertility
2. Helps reduce androgens (great for PCOS acne and hair loss)
3. May aid in natural weight loss

Ashwagandha for PCOS
1. Helps balance cortisol (stress hormone)
2. Supports thyroid function and energy
3. Assists in managing hyperandrogenism naturally

Omega-3 Fatty Acids
1. Fights inflammation
2. Improves insulin sensitivity
3. Helps with acne and mood swings

Spearmint Tea or Extract
1. Reduces testosterone naturally
2. Soothes bloating and improves digestion.
3. Can be part of your PCOS natural treatment routine

Vitamin D
1. Regulates periods
2. Improves mood
3. Supports weight loss and fertility

Magnesium
1. Supports blood sugar control
2. Helps manage anxiety and sleep
3. Balances hormones naturally
Zinc
1. Helps with acne and hair thinning
2. Supports insulin function
3. May reduce PCOS inflammation

Berberine
1. Naturally helps regulate blood sugar and insulin levels
2. Supports healthy weight management
3. Reduces inflammation and may help balance hormones
4. Improves cholesterol levels
How can Lifestyle changes help with PCOS?
Women with PCOS can significantly improve their symptoms through consistent lifestyle changes. While medication has its place, the right exercise approach can transform how you manage this condition.
Best Exercises for PCOS
Different exercise types offer unique benefits for PCOS management:
Cardiovascular Exercise
1. Enhances how your cells respond to insulin and boosts cardiovascular health
2. Try for 2.5 hours spread throughout your week at a moderate pace.
3. Consider gentle activities like pool sessions, casual bike rides, or neighborhood walks.
4. HIIT workouts compress effective training into shorter timeframes for busy schedules

Strength Training
1. Creates calorie-burning lean tissue that supports metabolism
2. Helps balance hormone levels and reshape body contours
3. Schedule 2-3 resistance sessions targeting all primary muscle areas each week
4. Particularly effective for reducing polycystic ovary syndrome belly fat.

Yoga and Mind-Body Practices
1. Surya namaskar (sun salutation) enhances circulation and hormone balance.
2. Reduces stress hormones that worsen PCOS symptoms
3. Supports better sleep quality
4. Can be practiced at home for PCOD recovery

Targeted Approaches for PCOS Concerns
How to Reduce PCOS Belly?
1. Combine Cardio and Core Exercises: Do 30-minute cardio intervals (e.g., jogging, cycling) 3 times weekly, paired with core-strengthening moves like planks and bicycle crunches (3 sets of 15 reps).
2. Engage Multiple Muscles: Try total-body exercises like squats or burpees to burn fat efficiently.
3. Stay Consistent: Moderate daily movement (e.g., 20-minute walks) is more effective than occasional intense workouts for reducing PCOS belly fat.
4. Manage Stress: High cortisol fuels abdominal fat. Practice deep breathing or yoga to lower stress; see our Brain Fog article.
How to Manage PCOS Weight?
1. Prioritize Consistency: Exercise 4-5 times weekly at a moderate pace (e.g., brisk walking, swimming) rather than high-intensity bursts.
2. Build Muscle: Strength training (e.g., lunges, push-ups, 2-3 sets of 10-12 reps) boosts metabolism by increasing lean muscle.
3. Track Non-Scale Progress: To stay motivated, measure waist size or energy levels, not just weight.
Evidence-Based Impact: Losing just 5% of body weight can improve symptoms like irregular periods and infertility (NHS)
What is the Best PCOS Treatment?
When it comes to PCOS treatment, medications are often the first line of approach to manage symptoms and improve quality of life. Although there is no definitive PCOS cure, the right treatment can effectively control symptoms, improve fertility, and prevent long-term complications.
Disclaimer: This article is for informational purposes only. Always consult a healthcare provider for your medical needs.
Medications For PCOS
Here’s a list of commonly used drugs for polycystic ovary syndrome treatment:
| Medication | Purpose |
|---|---|
| Metformin | A medication that enhances insulin sensitivity, supports more regular menstrual cycles, and can aid in managing weight. |
| Clomiphene (Clomid) | An oral fertility drug, often considered the first choice to induce ovulation, widely used as part of infertility treatments for PCOD. |
| Letrozole (Femara) | An aromatase inhibitor, preferred for ovulation induction, offering better pregnancy rates than Clomid in some cases. |
| Spironolactone | A prescription anti-androgen that helps manage hormonal acne and reduce excess facial and body hair associated with PCOS symptoms and treatment strategies. |
| Combined Oral Contraceptive Pills | Helps regulate periods, reduce androgen levels, manage acne, and lower the risk of endometrial hyperplasia. Widely used in polycystic ovaries treatment. |
| Eflornithine (Vaniqa) | A topical cream designed to slow the growth of unwanted facial hair, often used alongside other therapies for this condition. |
| Gonadotropins | Injectable hormones, used to induce ovulation in women who do not respond to oral medications. |
What are the PCOS Surgery options?
In cases where medication alone is insufficient, surgical interventions may be considered to manage polycystic ovary syndrome. The primary surgical option is ovarian drilling, a minor laparoscopic surgery aimed at improving ovulation and reducing androgen production.
Ovarian Drilling:
Procedure: Small holes are made in the ovaries using a laser or electrocautery during laparoscopy.
Purpose: To reduce androgen production (e.g., testosterone) and stimulate ovulation by altering the ovarian tissue
Indications: Typically recommended when first-line fertility treatments (e.g., clomiphene citrate) fail or in severe cases of anovulation (absence of ovulation)
Outcomes: This procedure can improve ovulation rates and increase the chances of pregnancy. Studies show that up to 47.4% of women may achieve pregnancy after the procedure, with many spontaneous conceptions.
Risks and Considerations: While generally safe, there are risks associated with surgery, including bleeding, infection, and potential damage to the ovaries. It should be considered only after careful evaluation and when other treatments have been unsuccessful
When To Seek Medical Help for PCOS?
If natural treatments like diet, supplements, and lifestyle changes fail to manage your symptoms, it may be time to seek medical help. Persistent symptoms can signal the need for professional care to address hormonal imbalances and prevent long-term health issues.
Who Can Diagnose PCOS?
Several healthcare providers can diagnose PCOD, depending on your needs:
1. Primary Care Physician: Conducts initial assessments, orders tests, and refers to specialists if needed.
2. Gynecologist: Specializes in women’s reproductive health and often diagnoses PCOS using medical history, physical exams, blood tests, or ultrasounds.
3. Endocrinologist: Focuses on hormonal disorders, ideal for complex PCOS cases involving insulin resistance or high androgen levels.
4. Reproductive Endocrinologist: Combines expertise in reproductive and hormonal issues, perfect for PCOS-related infertility.
